Now amidst the Omicron-wave of infections hitting vaccinated and unvaccinated alike, it is clear in our practice we are seeing a lot of exacerbations of sinus infections. COVID-19 often causes sinus and upper respiratory symptoms such as loss of smell, congestion, and a severe headache. However this leaves the susceptible person open to sinus infections and ear infections caused by bacteria that may last for several more weeks. Some patients of course are much more ill, with about 5 to 10% needing hospital care, and for those patients sinus infection or ear symptoms may go untreated for longer.
Patients with chronic sinusitis have complaints of nasal blockage, facial pressure, eye pressure, runny nose, postnasal drip and headache. COVID-19 is also causing loss of smell in most-if-not-all patients for a short time (some patients have been slow to recover). <<–Update! Omicron seems to cause LESS loss of smell due to reduced affinity for the nerve endings!
Persisting “sinus headache” affecting the frontal and ethmoid sinus areas (regions between the eyes and up onto the forehead) is the most common symptom following bacterial-negative COVID sinusitis. This may be present with runny nose as well, usually on both sides. But oddly about half of patients have no runny nose at this point. Some patients (about 10%) will have scalp tenderness, pain, and even sometimes PAINFUL HAIR! Pain at the top of the head is often found with occult sphenoid sinusitis, which can cause a serious infection of the eyes and even meningitis.
LOSS OF SMELL is happening in about 50% of patients with Delta Variant COVID. The loss of smell most commonly is resolved by 3 months, but about 20% of patients will have smell loss longer, and about 5% may have permanent loss of smell. OMICRON variant has seen reduced problems with smell loss!
OMICRON Original: Had much less loss of smell, but mostly sinus congestion symtpoms. There was a strong tendency toward SEVERE SORE THROAT and even GI upset moreso. Most of these patients retained their sense of smell and had disease course taht was brief – 3 days or so.
OMICRON VARIANT BA.2: These started popping up late December ’21. The Anosmia/smell dysfunction returned and I’m maybe even seeing this smell loss LAST LONGER than the original COVID variants. The severe sore throat is often still. Body aches and fatigue seem to linger longer. Most people were sick 6-9 days.
I have seen more patients with lingering sinusitis after Omicron COVID than prior variants. And the smell loss has been worse than the summer Delta surge. Omicron seems to be milder, but does seem to cause infections in many people with the vaccine. I do encourage you to get the vaccine and the booster. Depsite COVID Omicron being milder, January 2022 was one of the deadliest months our country has ever seen. Vaccination reduces your risk of COVID death 90% or more.
Patients with severe COVID migraine/headache phenomenon may also suffer from some chronic COVID brain symptoms (like “chemo brain” for patients receiving toxic chemotherapy). This may show up almost like non specific concussion symptoms with fatigue, mental fatigue, eye fatigue, non specific dizziness, feeling dizzy in wide open places, or feeling dizzy in busy indoor areas. Many patients with this kind of persisting head pain may benefit from migraine medications or those used to block neural signals upstream of nerve endings.
The nasal sinuses and the middle ear space or hollow pockets in the head and cranial bones that usually are filled with sterile air. However their natural ventilation tracts tracks can get blocked off allowing for nearby bacteria to take hold and cause painful swelling and infections. It is often patients who are susceptible to sinus infections that get them – such as those patients who have gotten them before or patients who had ear infections as a child. However really anyone is susceptible to sinusitis every once in a while.
Typically we allow 7 to 10 days for an acute sinus infection to resolve on its own, but after this point antibiotics or anti-inflammatories or other specialized medications may be needed. Common sinus infection bacteria are often Streptococcus species, Moraxella, or Haemophilus. Culture techniques or even PCR technology may be used to identify specific pathogens. However patients with a history of relapsing sinus infections may have more difficult bacteria such as Staphylococcus or very tricky non typical respiratory bacteria. Bacterial sinus infection secondary to COVID-19 may be a cause for lingering loss of smell. We’re hopeful that most people with COVID-19 regain their smell back, but unfortunately many do not.
If you are two weeks after your COVID-19 was diagnosed, and have recovered otherwise but need a visit for sinus evaluation, call us today. You are not the only one!
I have started using montelukast orally post-covid to help block leukotriene cytokine response in the covid sinus patients.
Dr. Rogers is an otolaryngologist in the Atlanta Georgia (USA) area since 2005 and specializes in seeing chronic sinusitis patients and patients with chronic nasal allergy complaints. Click for More Info about Dr. Rogers and how we can help out!
OTHER COVID-RELATED PAGES HERE:
Time For a Third Dose?
On Friday Sep 17th 2021 The FDA Advisory Panel made new recommendations about a third [...]
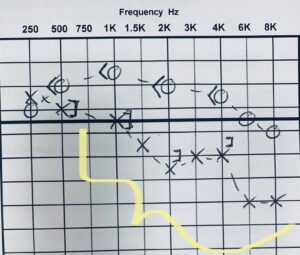
Read MoreCoronavirus-Related Hearing Loss
COVID and Hearing Health Most otolaryngologists will agree that hearing complaints are on the rise [...]
Read More